Persistent Pelvic Pain
Persistent (chronic) pelvic pain is a very common medical problem that will affect up to 1 in 5 women in their lifetime. Many will find this statistic very surprising, but it is, unfortunately, a stark reality that has a major effect on up to 20% of women’s ability to live a “normal” life. Dr Wynn-Williams has extensive experience in managing persistent pelvic pain in Australia – both in public and private practice.
Pelvic pain is invisible, and there is no easy way to recognise that someone is suffering from pelvic pain. Pelvic pain is one of the most common reasons for women to take time off from work or education. Persistent Pelvic Pain or Chronic Pelvic Pain is defined as intermittent or constant pain in the lower abdomen or pelvis – pain of at least six months duration, which does not occur exclusively with periods or during sex.
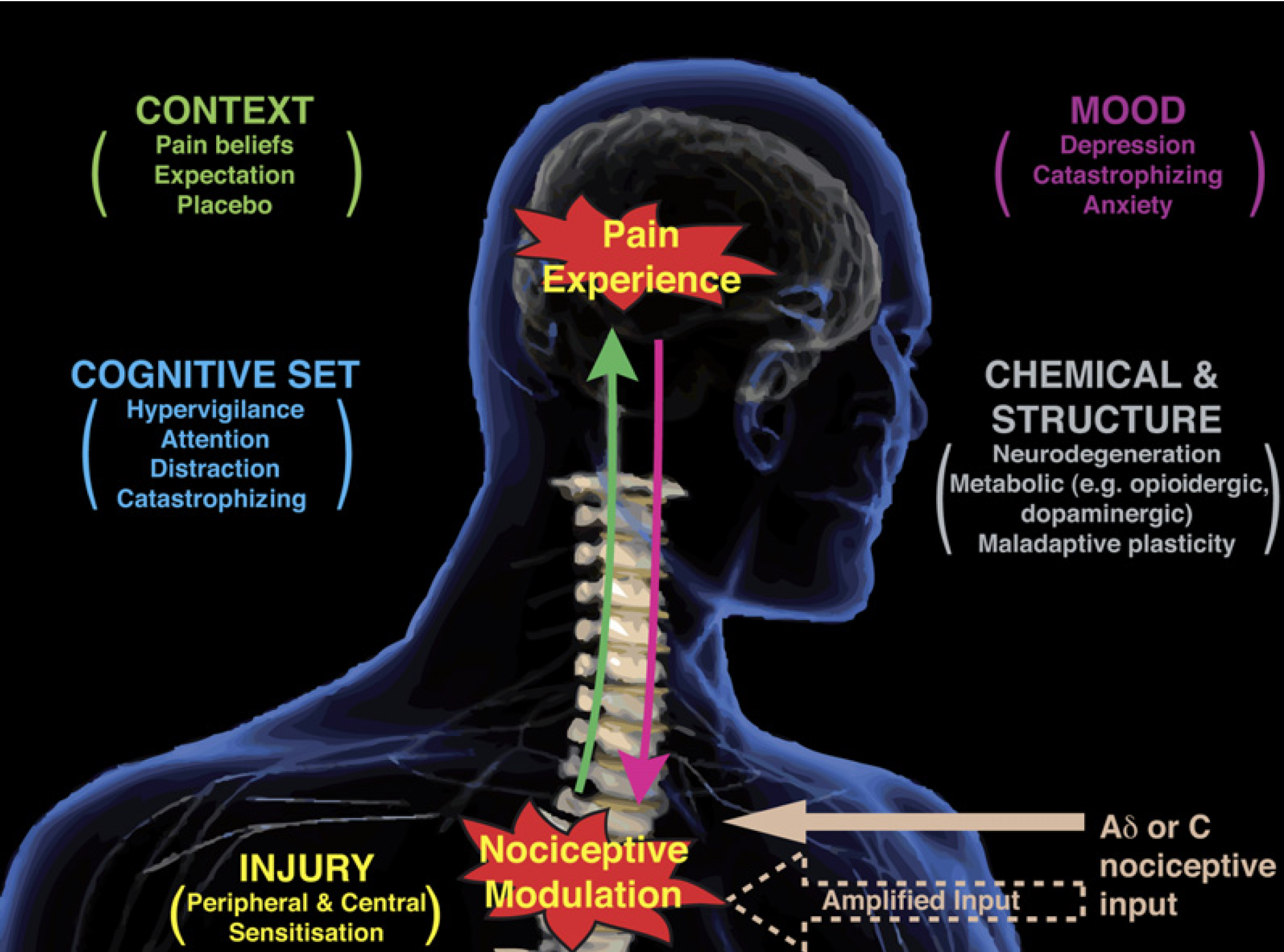
We don’t know why some women develop persistent pelvic pain, but we know that it often starts in their teens or twenties – with regular pain associated with their periods. Young women will find that other women in their family will have similar symptoms, and they learn that it is “normal” for the “women of the family”. They will often be told by friends, family, and their health professionals that it is normal and that nothing can be done. In these early years, the nervous system is still developing and can be susceptible to significant pain episodes. This attitude towards your pain can potentially have long-term effects.
Pelvic pain can have many causes, all affecting the structures in the pelvic or lower abdomen. One of the most common causes, affecting 1 in 10 women, is endometriosis. Endometriosis can cause pain before, during, and after the period, or at any time during the menstrual cycle. Some women with endometriosis have no pain symptoms. Other causes include abnormal hormone production in the lining of the wall in the first year or so of starting periods (primary dysmenorrhoea); adenomyosis, which could be described as endometriosis in the muscle of the uterus; and, issues with the bones, muscles, or nerves of the pelvis. Sometimes no obvious cause of the pain is found.
While some women with endometriosis will only ever have painful periods, others develop more complex pain over time, including any or all of the following pains:
Painful periods (Dysmenorrhoea)
Pelvic muscle pain causing painful intercourse (Dyspareunia); pain with smear tests or pain using tampons; pain on sitting, standing, or walking.
Bowel pain, bloating, cramps, and irritable bowel.
Pain opening bowels (Dyschezia)
Bladder symptoms of frequent voiding (Frequency), getting up at night (Nocturia), needing to get to a toilet in a hurry (Urgency), or flare-ups that feel like a urine infection.
Sharp, shooting or burning pains.
Frequent headaches or migraines.
Anxiety or depression.
Some women have one or more of these pains without having endometriosis.
If you are struggling with pelvic pain that has become more complicated than just simple period discomfort or you have had surgery for endometriosis, but still experience significant pain, it may take more than one health professional to help you be as well as you can be. Dr Wynn-Williams works with a multidisciplinary pelvic pain team that is dedicated to helping you master and control your pelvic pain.
As well as Dr Wynn-Williams, your pain team may include a pain specialist, your GP (general practitioner), psychologist, specialist pelvic physiotherapists, and nursing professionals, among others. Dr Wynn-Williams’ team can work with you to provide medical pain management approaches as well as help you develop the knowledge and skills for pain self-management that you can use on a daily basis.
Dr Wynn-Williams can offer a number of interventions including ensuring that the correct diagnosis has been made, pain education, medical management, pelvic floor botox and pudendal block, and the coordination of your pain team with referral to the appropriate health professionals. Unfortunately, women will often end up with repeat visits to emergency departments and have multiple operative or laparoscopic procedures because of persistent pelvic pain. Dr Wynn-Williams' aim is to help you break the cycle of pain and help you to live your life to the fullest.
Dr Wynn-Williams recommends that all his patients read “Endometriosis and Pelvic Pain” by A/Prof Susan Evans.